By a former insurance company attorney, who now fights for the claimant - Price McNamara If an insurance company denies your claim for accidental death insurance or life insurance benefits for the loss of a loved one claiming that “intoxication” or “driving while intoxicated” caused the death, do not give up. That’s exactly what they want you to do, even though you may be legally entitled to recover full benefits. No matter how long someone pays insurance premiums to protect their family, insurance companies care about profits, and paying claims doesn’t help with their profits. Fortunately, appealing the claim properly to the insurance company (known as an “administrative appeal”), and filing a lawsuit in federal court can result in your denied claim being approved for full benefits. The court can even award you your attorney fees for having to fight an unfair denial of benefits. ASK ANY LIFE INSURANCE OR ACCIDENTAL DEATH AND DISMEMBERMENT INSURANCE OR LIFE INSURANCE ATTORNEY. UNFAIR BENEFIT DENIALS BASED ON INTOXICATION EXCLUSIONS ARE RAMPANT. It could happen to you. It’s happened to many of my clients before they retained a lawyer. Good people, family breadwinners, pay insurance companies thousands of dollars for years to protect themselves and their loved ones against financial ruin in the event of their death or disability. Then when tragedy does strike, and families desperately need the benefits, the insurance companies cheat to issue grossly unfair claim denials base on an “intoxication” exclusion or other exclusions when the facts don’t support it. They’ll even illegally withhold key evidence as CIGNA recently did to issue a bogus claim denial to my client. So they profit and thrive while abandoning families to financial disaster. The saddest part is they often get away with it. Whether it’s a claim for life insurance or accidental death insurance benefits, don’t expect the insurance company to play fair. It won’t. It will pretend to befriend you while secretly plotting to build a case to avoid paying what you deserve. So brace yourself, you have entered an insurance war zone by daring to make a claim.
Table of Contents
What Does The Typical Accidental Death Insurance Policy Intoxication Exclusion Looks Like In Your Policy?
 The exact language of intoxication exclusion clauses in life insurance and accidental death and dismemberment insurance policies will vary from policy to policy. But the typical intoxication exclusion will read something like the one CIGNA recently tried to say barred recovery for my client whose husband died in a car crash (the full story follows below).
It stated:
The exact language of intoxication exclusion clauses in life insurance and accidental death and dismemberment insurance policies will vary from policy to policy. But the typical intoxication exclusion will read something like the one CIGNA recently tried to say barred recovery for my client whose husband died in a car crash (the full story follows below).
It stated:
“COMMON EXCLUSIONS
In addition to any benefit-specific exclusions, benefits will not be paid for any Covered Injury or Covered Loss which, directly or indirectly, in whole or in part, is caused by or results from any of the following unless coverage is specifically provided for by name in the Description of Benefits Section:…
5. the Covered Person’s intoxication as determined according to the laws of the jurisdiction in which the Covered Accident occurred;
6. voluntary ingestion of any narcotic, drug, poison, gas or fumes unless prescribed or taken under the direction of a Physician and taken in accordance with the prescribed dosage.”
Why Do Insurance Companies Get Away With Such Unfair Benefit Denials?
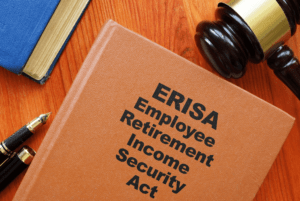
The insurance companies often get away with unfair claim denials because of “ERISA”, short for the federal law known as the “Employees Retirement Income Security Act.” ERISA law governs the vast majority of insurance contracts issued to employees as part of their employment benefits, whether it’s health, disability, life or accidental death insurance. This means that anyone who files suit because of a denied claim must do so in federal court. Most people have never even heard of ERISA unless they have endured the horrible experience of an insurance company, like CIGNA in the case described below, effectively declaring war with them for daring to seek the death or disability benefits they paid for and deserve. To make matters worse the very nature of these benefits always means the claimant victims must fight the war in the midst of a major personal and financial crisis that comes with losing a loved one. Although ERISA was enacted to protect claimants’ rights, in reality and in practice, it actually gives insurance companies the upper hand over the victim pursuing a claim for insurance benefits.A Story About Tragedy, Justice, and How to Beat Insurance Companies at Their Own Unfair Intoxication Exclusion Benefit Denial Game.
 My client, a young wife, survived this horrendous accident. Unfortunately her husband, who was driving, did not.
Can you imagine CIGNA insurance company withholding critical evidence from a grieving widow to help it unfairly argue that an intoxication exclusion clause voided coverage under her husband’s accidental death and dismemberment insurance policy? That’s exactly what CIGNA did to avoid paying over $1,000,000 in accidental death and dismemberment insurance benefits it owed to the young widow after her husband paid years of premium to protect her financially if something like this ever happened.
But a federal appeals court slammed CIGNA for doing it, and ordered CIGNA to pay it all.
My client, a young wife, survived this horrendous accident. Unfortunately her husband, who was driving, did not.
Can you imagine CIGNA insurance company withholding critical evidence from a grieving widow to help it unfairly argue that an intoxication exclusion clause voided coverage under her husband’s accidental death and dismemberment insurance policy? That’s exactly what CIGNA did to avoid paying over $1,000,000 in accidental death and dismemberment insurance benefits it owed to the young widow after her husband paid years of premium to protect her financially if something like this ever happened.
But a federal appeals court slammed CIGNA for doing it, and ordered CIGNA to pay it all.
Shattered Newlywed Bliss
Life as my client knew it changed forever after what began as a pleasant afternoon drive with her husband. Beautiful weather. They were newlyweds. He had a great job and often worked overseas, and they were inseparable when he was back home. She was reaching over to the backseat to play with the family dog who was along for the ride as they approached a gradual curve in the road. Her husband, who was driving, briefly turned to look. Just as they both looked back up, they saw the eighteen-wheeler coming head-on toward them. In his brief moment of distraction, her husband had continued driving a straight path when the road curved, sending them into the oncoming truck’s path. Suffering multiple bad injuries herself, it was a miracle my client survived the fiery crash at all. What was left of the car was hardly even recognizable. Tragically, her husband died in the hospital from massive injuries a few days later. It was an indescribable gut-punch. She was slowly recovering physically, but lost, scared and incredibly alone. While no great consolation, at least her late husband, the sole breadwinner, had paid for a very expensive accidental death and dismemberment insurance policy with CIGNA to protect her from exactly such an event as this. At least, she thought, she would be OK financially in her grief.Citing ERISA, and a Policy Exclusion for Intoxication, Cigna Denies the Widow’s Claim for Insurance Benefits
Imagine the bewildered widow’s shock when she opened CIGNA’s denial letter explaining that her claim was governed by the little known federal law known as ERISA, and that it refused to pay her insurance benefits, claiming her husband was intoxicated. CIGNA claimed that her husband’s blood and urine samples proved he was intoxicated at the time of the crash, and that the accident report stated he was “impaired.” The insurance policy excluded coverage for accidents caused by an insured’s intoxication. A second gut-punch. She was still recovering mentally and physically, she was broke, and felt like she was swirling the drain. But no way in the world was he impaired. There was no doubt in her mind.Illegally Withholding Evidence: What Cigna Knew But Didn’t Tell the Widow
 What’s shocking is what CIGNA’s denial letter DIDN’T tell the widow when it denied her claim.
GIGNA’s denial letter didn’t tell her that it had hired an expert toxicologist to review her husband’s blood and urine samples. The expert gave GIGNA a written report that the samples COULD NOT support a determination of intoxication. In other words, CIGNA’S own expert directly contradicted what it told my client to support its denial of her claim.
CIGNA’s denial letter also didn’t tell her that the original accident report didn’t even say “impaired”. Rather, the original report was amended more than six months after the accident to say “impaired” only after a telephone calls from CIGNA to state police prompted the amendment. This was long after her husband had died, and just seven days after CIGNA received its toxicologist’s report that a finding of impairment COULD NOT be supported.
So now CIGNA had something it could say in its denial letter to support its decision – the police report now said “impaired”. CIGNA issued its claim denial letter soon afterward. The letter talked all about the police report saying “impaired”. Of course it made no mention of its own toxicology expert’s opinion that impairment could not be determined.
What’s shocking is what CIGNA’s denial letter DIDN’T tell the widow when it denied her claim.
GIGNA’s denial letter didn’t tell her that it had hired an expert toxicologist to review her husband’s blood and urine samples. The expert gave GIGNA a written report that the samples COULD NOT support a determination of intoxication. In other words, CIGNA’S own expert directly contradicted what it told my client to support its denial of her claim.
CIGNA’s denial letter also didn’t tell her that the original accident report didn’t even say “impaired”. Rather, the original report was amended more than six months after the accident to say “impaired” only after a telephone calls from CIGNA to state police prompted the amendment. This was long after her husband had died, and just seven days after CIGNA received its toxicologist’s report that a finding of impairment COULD NOT be supported.
So now CIGNA had something it could say in its denial letter to support its decision – the police report now said “impaired”. CIGNA issued its claim denial letter soon afterward. The letter talked all about the police report saying “impaired”. Of course it made no mention of its own toxicology expert’s opinion that impairment could not be determined.
The Long Path to Justice Under ERISA Law
Our client’s claim illustrates the typical procedural path for claims for insurance benefits governed by ERISA law after the insurance company initially denies a claim.Cigna Denies the Administrative Appeal, Continuing to Withhold the Critical Toxicology Evidence
CIGNA persisted in its denial of benefits throughout the “administrative appeal” process required by ERISA law. The administrative appeal is where the insurance company basically takes a second look at its own initial claim denial. Throughout the process, CIGNA still never disclosed its toxicologist’s report despite written request on my client’s behalf for any such document. ERISA requires an insurance company who denies a claim to produce all evidence from its investigation to a claimant who requests it. But the insurance companies will sometimes withhold documents they are required to produce if the documents don’t support the denial of benefits.The Federal District Court Lawsuit for Denial of ERISA Insurance Benefits-The Evidence Cigna Withheld Finally Comes to Light
ERISA law doesn’t allow a claimant to file a lawsuit until after taking an administrative appeal with the insurance company, which usually just results in another denial of benefits. So after CIGNA denied the administrative appeal, we filed suit in federal district court for wrongful denial of ERISA accidental death insurance benefits. CIGNA chose to hire and pay several attorneys from a large corporate law firm to fight against paying the widow’s claim. For the first time, CIGNA, through its attorneys, produced a stack of more than 1000 pages of documents from its investigation, never produced before. Its toxicology expert’s critical report, just a few pages long, was buried deep within it. We presented this newly-revealed report to the unbiased Coroner, the physician who actually signed my client’s husband’s death certificate, and asked him for his opinion. The Coroner gave us a sworn statement, testifying in agreement with CIGNA’s own toxicologist, that the blood and urine samples could not support a finding of intoxication or impairment. At that point, we hoped and really thought that reason would prevail once we shared this with CIGNA. We pointed out to CIGNA what its own expert and the Coroner said about impairment and intoxication, but even this didn’t change CIGNA’s mind. Remember, paying claims, whether legitimate or not, doesn’t help insurance company profits. CIGNA’s thought must have been that paying its attorneys to fight the court battle, if they could win, would be less expensive than paying benefits to a deserving claimant. Believe it or not, citing ERISA legal technicalities, CIGNA’s lawyers told us that CIGNA wouldn’t even consider the unbiased Coroner’s affidavit because it had already completed its investigation. CIGNA’s attorneys then actually argued against letting the judge even consider the affidavit as evidence at trial. The attorneys cited to the ERISA technicality that the court can’t consider evidence that was not presented to the insurance company to consider during the administrative appeal process. So we took the case to trial, but to my client’s dismay, the district court judge ruled in favor of CIGNA and against my client citing technicalities of ERISA law. A third gut punch.Justice Prevails, Finally, on Appeal to the U.S. Fifth Circuit Court of Appeal
Although discouraged, our client let us continue the fight. Still firmly convinced that she was deserving and entitled to her benefits, we appealed the district court’s decision to the U.S. Fifth Circuit Court of Appeal, which is responsible for reviewing the decisions of all federal district courts in Texas, Louisiana and Mississippi. There she finally received well-deserved justice. The Fifth Circuit reversed the district court in favor of this wonderful, brave and spiritual lady, ruled that CIGNA (Life Insurance Company of North America) must pay her claim. In other words, the court held that CIGNA’s intoxication exclusion didn’t apply, and delivered a clear message to insurance companies: While insurance companies often get away with unfair claim denials under ERISA law, they will not get away with ignoring, or worse, like CIGNA did here, withholding key evidence to justify an abusive claim denial. The Court explained (quoting from the Fifth Circuit’s written opinion of public record):“LINA did not provide [its toxicologist’s] report to [redacted]…Importantly, although the letters of denial relied entirely on the toxicology results, the death certificate, and the amended collision report (which included the DWI citation), neither of LINA’s denials of coverage mentioned [the toxicologist’s] report…For the first time, [redacted] discovered [the] report in the documents LINA filed with the court…Thus, we consider LINA’s actual withholding of [the] report from [redacted]. [redacted] argues that LINA’s failure to provide her with [the] report, despite her written request for “any and all documents” LINA would “rely on toward making [its] decision,” violated ERISA’s procedural rules and thus denied …[redacted] a “full and fair review.”…Contrary to LINA’s assertions, [the] report undermines LINA’s position that intoxication or drug abuse was the cause of [redacted] death. Further, this opinion comes from the report of LINA’s very own expert. As such, without [the] report, during the administrative process [redacted] was unable to meaningfully challenge LINA’s finding that [redacted] death was caused by intoxication or drug abuse. We therefore conclude that LINA did not substantially comply with ERISA’s procedural requirements and, consequently, denied [redacted] a “full and fair review.”…
In sum, taking into account LINA’s conflict of interest, its procedural unreasonableness, its denial of a full and fair review, and the counter-balanced nature of the evidence, we hold that LINA abused its discretion in denying benefits… Accordingly, we reverse the district court’s judgment. We remand with instructions to enter judgment in favor of [redacted] and for such further proceedings as may be necessary and fully consistent with this opinion.
REVERSED and REMANDED.”
A Perfect Example of Why to Never Give up When the Insurance Company Claims the Intoxication Exclusion Bars Your Claim
 My client’s maddening story shows just how far insurance companies will go to deny a claim. It also illustrates how the insurance companies exploit the huge legal advantage given to them by many features of ERISA’s stacked (in their favor) deck. They often refuse to give in, and choose to hire attorneys, thereby forcing claimants to hire attorneys as well, until the court ultimately orders them to pay.
But her story also demonstrates that you should never just accept a life insurance or accidental death insurance company’s denial of benefits based on any policy exclusion as honest or legally correct. Justice can prevail despite the brutality of ERISA law. At the end of her legal battle, the Fifth Circuit’s written opinion delivers a clear message to insurance companies: While insurance companies often get away with unfair claim denials under ERISA law, they will not get away with ignoring, or worse, like CIGNA did here, withholding key evidence to justify a claim denial.
My client’s maddening story shows just how far insurance companies will go to deny a claim. It also illustrates how the insurance companies exploit the huge legal advantage given to them by many features of ERISA’s stacked (in their favor) deck. They often refuse to give in, and choose to hire attorneys, thereby forcing claimants to hire attorneys as well, until the court ultimately orders them to pay.
But her story also demonstrates that you should never just accept a life insurance or accidental death insurance company’s denial of benefits based on any policy exclusion as honest or legally correct. Justice can prevail despite the brutality of ERISA law. At the end of her legal battle, the Fifth Circuit’s written opinion delivers a clear message to insurance companies: While insurance companies often get away with unfair claim denials under ERISA law, they will not get away with ignoring, or worse, like CIGNA did here, withholding key evidence to justify a claim denial.
The Big Question: Why Did This Case Go so Far Since It Seemed Clear That the Insurance Company Should Pay?
THE SIMPLE ANSWER: ERISA . Actually it happens all the time, and nationwide. ERISA controls the vast majority of employer-provided benefits throughout the country, including life insurance, accidental death and dismemberment insurance and short and long-term disability insurance. Although ERISA was enacted to protect claimants’ rights, in reality and in practice, it actually gives insurance companies the upper hand over the victim pursuing a claim for insurance benefits. The insurance companies exploit the huge legal advantage given to them by the following features of ERISA’s stacked deck. THE INSURANCE COMPANY’S INHERENT CONFLICT OF INTEREST. The unfairness of ERISA begins with an initial claims process wracked with conflicts of interest. When a victim makes a claim, the initial decision to pay or deny it is almost always made by the insurance company itself, who obviously loses money by paying and profits from denying claims. After all, an insurance company’s entire business model is to maximize receipt of premium payments received from their insureds who think they’re buying protection, while minimizing what it pays in claims. Who wouldn’t expect rampant abuse in the form of unjust million dollar claim denials under such a model? ERISA’S FAULTY ADMINISTRATIVE APPEAL PROCESS. If the insurance company initially denies the claim, a typical result, ERISA prohibits the claimant from filing a lawsuit until completing what the insurance company calls an “independent” administrative appeal. But who then decides whether to uphold or overturn the original denial at the administrative appeal level? You guessed it – the same insurance company. By “independent”, they simply mean different claims personnel of the same insurer that initially denied the claim. Do you think the claims personnel know the result their insurance companies, who write their paychecks want? The typical result is denial of the claim on administrative appeal.Two Ways That ERISA Effectively Ties the Hands of Federal Judges Who Want to Be Fair
FIRST, ERISA RESTRICTS THE EVIDENCE A FEDERAL COURT CAN CONSIDER AT TRIAL. After the insurance company denies the administrative appeal, ERISA allows the victim to file suit in federal district court. A federal district court judge ultimately conducts a “trial”, but one which is different than what most people would picture. Unlike most lawsuits, ERISA suits are not tried before a jury. Nor do any live witnesses testify. Instead, the trial evidence is limited to the “administrative record”. That is, the judge is only permitted to consider the same evidence the insurance company reviewed in the process of denying the claim. The actual administrative claim file is filed into the court record, and attorneys representing the victim and the insurance company file trial briefs arguing the merits of their respective clients’ cases in light of ERISA law and the evidence in the administrative record. The district court judge reviews all of this, may or may not allow the attorneys to give oral arguments, and issues an opinion and judgment for either the insurance company or the claimant. What this means for the claimant, is that the initial claim and administrative appeal process is critical to success. If he or she does not present important evidence to the insurance company during the initial claim or administrative appeal, the court is generally prohibited from considering it at trial. ERISA law can require that the judge completely disregard even evidence that it considers critical or outcome determinative if presented at trial if it was not made part of the administrative record before the claimant files suit. For that reason, handling the initial claim and administrative appeal process properly before filing suit is crucial. The claimant’s ERISA attorney’s job is to assure that ALL evidence conceivably helpful to the claimant is gathered and made part of the administrative record before filing suit. Otherwise the judge cannot consider it when the case inevitably lands in court after the insurance company denies the claim. SECOND, ERISA’s “STANDARD OF REVIEW” CAN FORCE JUDGES TO UPHOLD CLAIM DENIALS EVEN WHEN THEY THINK THE INSURANCE COMPANY WAS WRONG. In addition to ERISA’s constraints on the courts’ consideration of evidence, ERISA law in most cases requires that the court give “deferential review” to the insurance company’s decision to deny a claim. This often means that a judge must uphold a denial even if he or she thinks the insurance company was wrong, and even if he or she would have ruled the other way. It’s not uncommon for a judge to expressly state in a written opinion that he or she believes the insurance company was wrong for denying a claim, and that the judge would have ruled differently, but must rule in the insurance company’s favor because of ERISA’s deferential “standard of review”.Why Do so Many Deserving Claimants End up With Nothing, Even When an Insurance Company Unfairly Denies a Life or Accidental Death Insurance Claim Based Upon an Intoxication Exclusion in the Policy?
Many deserving claimants, who absolutely should have been paid, are swindled out of hundreds of thousands or even millions of dollars in insurance benefits based on the intoxication exclusion. The sad thing is, those benefits were meant as financial protection that their loved ones paid for and wanted them to have. These swindled claimants largely fall into three categories: 1.) Those who trust that the insurance company’s denial is correct; 2.) Those who think a denial is unfair, but don’t believe that they can beat big insurance companies, so they just give up; and 3.) Those who try to fight an unfair intoxication exclusion clause defense without the help of an experienced ERISA attorney. The insurance companies, of course, love claimants who fall into these three categories.Many People Just Assume the Insurance Company Is Being Honest With Them, and Just Accept the Denial as Proper
Many deserving claimants just trust that the insurance company’s denial is correct. Insurance companies know this, and deny legitimate claims knowing that they’ll get away with many denials because honest claimants wrongly assume the insurance company is honest too. The insurance companies’ claims personnel are well trained to display empathy and compassion to the claimant during all communications to build trust. This leads many to accept unfair denials and go away without even attempting to seek an attorney’s advice, take an administrative appeal or file a lawsuit.Many People Who Think a Denial Is Unfair Don’t Believe That They Can Beat Big Insurance Companies, so They Just Give Up
Many people understandably feel that if they choose to fight a claim denial, the insurance companies will win. After all, big insurance companies do have seemingly unlimited resources, and hire some of the biggest law firms in the country to represent them in court. And the claim and administrative appeal process can be time consuming, and require legal expertise to handle properly. This is especially true if the case ends up in federal court. So many claimants, even if they believe a claim denial is bogus, still give up and go away without attempting to seek an attorney’s advice, take an administrative appeal or file a lawsuit.Many People Try to Fight a Claim Denial Alone, Without the Help of an Attorney
Many people understandably believe that if they make a well-reasoned argument to the insurance company on administrative appeal, the insurance company will “see the light,” be fair, reverse the denial and pay benefits. Where most claimants lose, without knowing it, is during the administrative appeal process. The way most claimants lose here is by failing to assure that ALL evidence conceivably helpful to the claimant is gathered and properly made part of the administrative record during that process before filing suit. The fatal result is that the judge cannot consider any evidence gathered later when the dispute inevitably lands in federal court after the insurance company denies the claim on administrative appeal.Why an Experienced ERISA Attorney Is Advised for Fighting an Insurance Company’s Intoxication Exclusion Clause Defense in a Life or Accidental Death Insurance Claim
 As a practical matter, an insurance claimant fighting an ERISA life or accidental death insurance intoxication clause denial on administrative appeal or in court without the help of a seasoned ERISA attorney is ill-advised. But that doesn’t mean you can’t win. It just means you may need help.
The reason an ERISA attorney’s help is advised is that ERISA law is complex, and some of the arguments you need to make to be successful are very technical.
The legal battle in an ERISA case, done right, can also be very tedious and time-consuming. The fight requires a ton of work from the time of the insurance company’s initial denial, through the administrative appeal process, through judgment at the district court level, then finally through judgment at the appeal court level. And the insurance companies typically hire several attorneys who specialize in ERISA law from some of the largest law firms in the country to fight the claimant’s attorney every step of the way.
Our client’s case, summarized above, is a perfect example of the amount of work that can be required to beat an insurance company who argues an intoxication defense. We took a loss on administrative appeal to CIGNA. Then we took another loss at the district court level, meaning the district court judge agreed with CIGNA’s lawyers on the intoxication exclusion defense.
It wasn’t until after taking an appeal to a three-judge panel of the U.S. Fifth Circuit Court of Appeal that my client finally received justice. All told, bringing our client’s case to a successful conclusion took hundreds of hours of work in researching and briefing the facts from an administrative record over 1000 pages long. It took finding the one critical toxicologists report that CIGNA first withheld, buried deep in that record. It took meeting with the Coroner to secure his testimony clarifying his comment made on the death certificate. It took researching and arguing the law to four judges in two separate court proceedings. And at the formal Fifth Circuit court hearing (called “oral argument”), where the attorneys make their arguments in open court to the judges, who pepper them with questions, comments and arguments about their positions, it was hard to tell whose position the judges actually favored. It was certainly nerve-racking for our client, who watched it. It wasn’t until the Court’s formal opinion landed in our email inbox a couple of months later that we could tell our client the good news.
As a practical matter, an insurance claimant fighting an ERISA life or accidental death insurance intoxication clause denial on administrative appeal or in court without the help of a seasoned ERISA attorney is ill-advised. But that doesn’t mean you can’t win. It just means you may need help.
The reason an ERISA attorney’s help is advised is that ERISA law is complex, and some of the arguments you need to make to be successful are very technical.
The legal battle in an ERISA case, done right, can also be very tedious and time-consuming. The fight requires a ton of work from the time of the insurance company’s initial denial, through the administrative appeal process, through judgment at the district court level, then finally through judgment at the appeal court level. And the insurance companies typically hire several attorneys who specialize in ERISA law from some of the largest law firms in the country to fight the claimant’s attorney every step of the way.
Our client’s case, summarized above, is a perfect example of the amount of work that can be required to beat an insurance company who argues an intoxication defense. We took a loss on administrative appeal to CIGNA. Then we took another loss at the district court level, meaning the district court judge agreed with CIGNA’s lawyers on the intoxication exclusion defense.
It wasn’t until after taking an appeal to a three-judge panel of the U.S. Fifth Circuit Court of Appeal that my client finally received justice. All told, bringing our client’s case to a successful conclusion took hundreds of hours of work in researching and briefing the facts from an administrative record over 1000 pages long. It took finding the one critical toxicologists report that CIGNA first withheld, buried deep in that record. It took meeting with the Coroner to secure his testimony clarifying his comment made on the death certificate. It took researching and arguing the law to four judges in two separate court proceedings. And at the formal Fifth Circuit court hearing (called “oral argument”), where the attorneys make their arguments in open court to the judges, who pepper them with questions, comments and arguments about their positions, it was hard to tell whose position the judges actually favored. It was certainly nerve-racking for our client, who watched it. It wasn’t until the Court’s formal opinion landed in our email inbox a couple of months later that we could tell our client the good news.
What Does the Final Work Product That an ERISA Attorney Presents in Court to Fight a Life or Accidental Death Insurance Policy Claim Denial Based on an Intoxication Exclusion Look Like?
Most claimants have no real way to know what goes into researching, briefing and arguing an ERISA life or accidental death insurance intoxication exclusion case to the court. So to give claimants some real-world perspective, we’ve reproduced in full our opening brief and reply brief filed in our client’s case with the U. S. Fifth Circuit Court of Appeals below. If interested, you can also listen to the oral argument by clicking this link. Read the full court opinion for White v. Life Insurance Company of North America (CIGNA), 892 F.3d 762, 5th Cir.(La.), June 13, 2018, as revised (Jun 14, 2018).Cigna Went Too Far by Ignoring and Withholding Evidence in This Case
The Fifth Circuit’s judgment was a just ending for our deserving client, no doubt, but CIGNA should have simply paid the benefits it owed her without withholding critical evidence and putting her through a ridiculous fight. It would have saved court resources, attorney’s fees on both sides and much delay and distress for a grieving widow.What Will Stop ERISA Insurance Claim Denial Abuse?